The Lone Star State of Mind: A Comprehensive Analysis of Mental Health Access Challenges in Texas (2026)
As of January 2026, the mental health landscape in Texas presents a paradox: alongside this growth, a deepening crisis in behavioral health accessibility threatens the state's social and economic vitality profound economic prosperity and persistent systemic fragility. Texas remains the economic engine of the South, characterized by rapid population growth, a booming labor market, and expanding urban centers. Yet, parallel to this growth runs a deepening crisis in behavioral health accessibility that threatens the social and economic vitality of the state. This report, commissioned to provide a definitive analysis of the therapeutic market, illuminates the structural, financial, and geographic barriers that effectively ration mental health care to a privileged few, while leaving millions of Texans in a precarious state of unmet need.
The 2026 ecosystem is defined by a convergence of historical policy decisions and emerging environmental stressors. Texas continues to hold the unenviable position of ranking last—50th—in the nation for access to mental health care. This ranking is , profound economic prosperity,not merely a statistical artifact but a reflection of a system where 22% of adults remain uninsured, the highest rate in the United States. The refusal to expand Medicaid has crystallized a "coverage gap" that entraps over a million working-poor adults, effectively barring them from the therapeutic marketplace. Simultaneously, a severe workforce shortage has left 246 of the state's 254 counties designated as Mental Health Professional Shortage Areas (HPSAs), creating vast "mental health deserts" where care is geographically unattainable.
Beyond these familiar structural deficits, 2026 has brought new variables into sharp relief. The escalating impact of climate change, specifically the "heat dome" phenomenon, has been empirically linked to deteriorating mental health outcomes, introducing a new environmental determinant of health. Furthermore, the evolving opioid crisis, now exacerbated by the presence of xylazine in the drug supply, has outpaced the state's limited substance use treatment infrastructure.
This report offers an exhaustive examination of these challenges. It dissects the insurance labyrinth, analyzing disparities between fully insured and self-funded plans; maps the workforce crisis from the residency pipeline to rural retention; and explores the unique vulnerabilities of Hispanic populations, youth, and rural communities. By synthesizing data from state agencies, federal reports, and academic research, this document serves as both a status report and a strategic roadmap for understanding the formidable obstacles facing patients, providers, and policymakers in the Lone Star State.
The National Context and Texas Rankings
The 2025-2026 Scorecards: A Consistent Lag
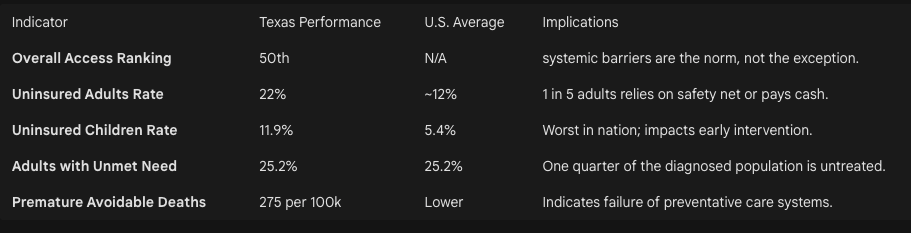
To understand the lived reality of a Texan seeking therapy in 2026, one must first engage with the macro-level data that defines the state's performance relative to the rest of the union. The metrics are unambiguous and concerning. Across every major scorecard evaluating health system performance, Texas consistently trails the vast majority of the United States, a trend that has calcified over the last decade despite incremental legislative efforts.
The 2025 State of Mental Health in America report, a benchmark publication for the industry, ranks Texas 50th for "Access to Care". This ranking is a composite measure that accounts for access to insurance, access to treatment, quality and cost of insurance, access to special education, and workforce availability. Being ranked 50th signifies that Texas is essentially the most difficult state in the country for a resident to navigate the mental health system. The report categorizes states ranked 39-51 as providing "relatively less access to insurance and mental health care," a cohort in which Texas is deeply entrenched.
This low ranking is a function of a "high prevalence, low access" dynamic. While the prevalence of mental illness in Texas is comparable to other large states—influenced by urbanization, economic stress, and social displacement—the mechanisms for addressing these illnesses are structurally deficient. The data indicate that states with higher rankings (1-13) have successfully integrated insurance access with workforce development, creating a safety net that captures those in crisis. In contrast, Texas’s system is characterized by porousness, where individuals fall through gaps created by cost, distance, and lack of providers.
The Commonwealth Fund Assessment
The Commonwealth Fund’s 2025 Scorecard corroborates the MHA findings, highlighting that the Texas health care system is structurally misaligned with thits population's needsundercountse needs of its population. The scorecard emphasizes that Texas has the highest rate of uninsured adults in the nation at 22%. This single statistic is the gravitational center of the mental health crisis. In a healthcare system predominantly driven by market rates and insurance reimbursement, lack of coverage is effectively a denial of service for all but the most acute, life-threatening emergencies.
The Scorecard further reveals that 25.2% of adults with any mental illness (AMI) in Texas report an unmet need for treatment. This figure, while stark, likely represents an undercount. "Unmet need" is a self-reported metric; it captures those who recognized they needed help and tried to get it but failed. It does not capture the "latent need" of individuals who, discouraged by stigma or the obvious lack of resources in their community, never attempted to seek care in the first place.
The "Uninsured Capital" of America
The moniker "Uninsured Capital" is not merely a derogatory label; it is the defining economic feature of the Texas mental health market. As of 2025, approximately 5 million Texans lack health insurance. To put this magnitude in perspective, the uninsured population of Texas exceeds the total population of 25 other U.S. states. This is not a marginal issue affecting a small subset of the poor; it is a mass-market reality affecting the working class, the gig economy, and the creative class.
The disparity is particularly glaring when compared to neighboring states. The Texas uninsured rate for adults aged 19-64 stands at 21.7%, which is nearly double the national average of 11.0%. Even within the region, Texas stands apart. Neighbors with different policy stances show significantly higher coverage rates: Louisiana (10.0%), Arkansas (12.4%), and New Mexico (13.3%). This stark regional contrast suggests that the crisis is not an inevitable outcome of geography or demographics, but a direct result of divergent policy choices.
The implications for mental health therapy are direct and devastating. Psychotherapy is a labor-intensive service with market rates in Texas urban centers typically ranging from $120 to $250 per session. For an uninsured individual, a standard course of Cognitive Behavioral Therapy (CBT)—often 12 to 16 sessions—would cost between $1,500 and $4,000 out of pocket. In a state where a significant portion of the population struggles with housing and food security, this cost barrier renders therapy a luxury good, accessible only to the wealthy or those fortunate enough to secure a spot in the limited sliding-scale clinics.
The Insurance Labyrinth
The financial architecture of mental health care in Texas is a complex labyrinth where the path to coverage is often blocked by high deductibles, narrow networks, and regulatory loopholes. Understanding this system requires dissecting the distinct experiences of the Medicaid population, the "coverage gap" population, and the privately insured.
The Medicaid Expansion Standoff
The defining policy decision of the last decade in Texas health care remains the refusal to expand Medicaid under the Affordable Care Act. As of 2026, the Texas Legislature has consistently voted down expansion measures, most recently in April 2025. This decision has created a unique and rigid stratification of access.
Texas Medicaid eligibility criteria are among the strictest in the United States. Coverage is largely restricted to children, pregnant women (up to one year postpartum), the elderly, and individuals with significant disabilities. Able-bodied adults, regardless of how low their income falls, generally do not qualify unless they are parents, and even then, the income threshold is draconian. A single parent in a family of three must earn less than approximately $4,000 annually to qualify for Medicaid coverage.
This threshold effectively excludes the entire working poor population. An individual working part-time at minimum wage earns too much for Texas Medicaid. However, because they earn less than 100% of the Federal Poverty Level (FPL), they do not qualify for subsidies on the federal Health Insurance Marketplace (HealthCare.gov). This entrapment is known as the "Coverage Gap."
In 2026, an estimated 1.1 million Texans fall into this gap. These are restaurant servers, childcare workers, construction laborers, and artists—the backbone of the Texas service economy. For these individuals, mental health care is practically non-existent. They cannot afford private insurance, they are ineligible for government aid, and they earn too little to pay out-of-pocket. The result is a deferred care model: mental health conditions are ignored until they precipitate a crisis, leading to emergency room visits or interactions with the criminal justice system, which effectively becomes the provider of last resort.
Private Insurance: The Illusion of Parity
For the roughly 50% of Texans who have employer-sponsored insurance or purchase plans on the marketplace, access to therapy is theoretically protected by the Mental Health Parity and Addiction Equity Act (MHPAEA). This federal law, mirrored by state regulations, mandates that insurance coverage for mental health and substance use disorders (MH/SUD) be no more restrictive than coverage for medical and surgical benefits.
However, in 2026, the promise of parity remains largely unfulfilled due to the prevalence of Non-Quantitative Treatment Limitations (NQTLs). Unlike quantitative limits (e.g., a cap on the number of visits), NQTLs are administrative barriers that are harder to police but equally restrictive.
The "Ghost Network" Phenomenon
The most pervasive NQTL in Texas is inadequate network design. Insurers maintain provider directories that appear robust on paper but are "ghost towns" in reality.
Inaccurate Directories: A patient may log into their insurer’s portal and see 50 psychiatrists listed within 10 miles. Upon calling, they often find that:
30% of the numbers are disconnected or wrong.
40% of the providers are no longer accepting new patients.
20% have left the network or the profession.
The remaining 10% have waitlists of 3-6 months.
Reimbursement Rates: The root cause of these ghost networks is low reimbursement. Insurance reimbursement rates for psychotherapy in Texas have not kept pace with inflation or the cost of practice operations. Consequently, many highly qualified therapists have opted out of the insurance system entirely, moving to a "private pay" or "cash only" model. This creates a two-tiered system where the best care is reserved for those who can pay cash and seek out-of-network reimbursement, while those reliant on in-network benefits face substandard access.
Medical Management and Prior Authorization
Insurers in Texas frequently employ aggressive medical management techniques for mental health. This includes "fail-first" protocols (step therapy), where a patient must fail on a cheaper medication or lower level of care before being approved for the treatment their doctor recommends. For example, a patient needing residential treatment for an eating disorder may be forced to fail at outpatient therapy first, a dangerous delay that can lead to medical instability.
Regulatory Jurisdictions: Fully Insured vs. Self-Funded
A critical distinction that confuses many Texas consumers is the difference between fully insured and self-funded health plans. This distinction determines which government agency has the power to protect them.
Fully Insured Plans: These plans are purchased by individuals or small businesses directly from an insurance company. The insurer assumes the financial risk. These plans are regulated by the Texas Department of Insurance (TDI). Consumers with "TDI" or "DOI" on their ID cards have recourse to state protections, state parity laws, and state complaint processes.
Self-Funded Plans: Most large employers in Texas (e.g., major tech companies, oil and gas firms, hospital systems) use self-funded plans. In this model, the employer pays the claims directly from their own funds, using an insurance company merely as an administrator (ASO). These plans are regulated by the federal government under ERISA (Employee Retirement Income Security Act) and are exempt from most state insurance laws.
Implication: Approximately 50-60% of insured Texans are in self-funded plans. When the Texas Legislature passes a new law mandating coverage for a specific mental health service or strengthening parity enforcement, it does not apply to the majority of Texans. This regulatory fragmentation leaves millions without the protections touted by state politicians, creating a false sense of security regarding coverage.
The Workforce Crisis – A State of Shortage
If insurance is the financial gatekeeper, the workforce is the physical bottleneck. In 2026, the supply of mental health professionals in Texas is critically insufficient to meet the demand generated by a population of over 31 million people. The shortage is not merely a matter of numbers; it is a crisis of distribution, diversity, and pipeline development.
The Geography of Scarcity: HPSAs
The federal Health Resources and Services Administration (HRSA) designates areas with a critical lack of providers as Health Professional Shortage Areas (HPSAs). The metrics for Texas in 2026 are alarming.
Near-Total Coverage: As of 2025, 246 out of Texas's 254 counties were wholly or partly designated as mental health HPSAs. This means that 97% of the state's geography is officially classified as underserved.
The Ratio Gap: To be considered adequately served, a region typically needs a population-to-psychiatrist ratio of 30,000:1. In many Texas counties, this ratio is effectively infinite because there are zero providers. In others, it exceeds 100,000:1.
The shortage is most acute in the rural Panhandle, West Texas, and the Border region. In these areas, the "mental health system" often consists solely of law enforcement and primary care. Residents experiencing a psychotic break or severe depressive episode have no local specialist to turn to. They are often transported by police to the nearest emergency room, which may be hours away, and then wait days for a bed in a state hospital.
The Provider Pipeline Problem
The shortage is driven by a structural failure to produce and retain enough professionals to keep pace with population growth.
Educational Bottlenecks: While Texas has expanded its medical schools, the number of psychiatry residency slots has not grown proportionately. A medical student may graduate in Texas but be forced to leave the state for residency training due to a lack of positions. Research shows that doctors tend to practice where they complete their residency, meaning Texas effectively exports its talent.
Licensure Hurdles: For non-physician providers like Licensed Clinical Social Workers (LCSWs) and Licensed Professional Counselors (LPCs), the path to licensure is arduous. It requires a master's degree followed by 3,000 hours of supervised clinical practice. During this internship phase, candidates are often unpaid or underpaid, creating a financial barrier that disproportionately filters out low-income and minority candidates.
Distribution of Social Workers: While the number of LCSWs has grown by nearly 50% over the last decade, they are heavily concentrated in the "Texas Triangle" (DFW, Houston, Austin, San Antonio). 91 counties in Texas have zero LCSWs. This means that in over a third of the state, there is no one licensed to provide advanced clinical social work services, which are often the backbone of community mental health.
The Role of Primary Care and Collaborative Care
Given the specialist shortage, the burden of mental health care falls disproportionately on Primary Care Providers (PCPs). It is estimated that up to 70% of mental health care in Texas happens in primary care settings.
The Collaborative Care Model (CoCM): The Meadows Mental Health Policy Institute has championed the CoCM, which integrates behavioral health into the primary care workflow. In this model, a PCP manages the patient with the support of a case manager and a remote psychiatric consultant. This leverages the scarce time of psypsychiatrists' scarce time, allowing them to oversee the care of a largchiatrists, allowing them to oversee the care of a massive panel of patients rather than seeing them 1:1.
Challenges: While effective, adoption is slowed by billing complexities. Many PCPs in rural Texas are already overwhelmed and lack the administrative bandwidth to implement new integrated care systems without significant technical assistance and financial incentives.
Innovative Workforce Solutions: Peer Support
In response to the clinician shortage, Texas has increasingly turned to Peer Support Specialists. These are individuals with lived experience of mental illness or substance use recovery who are trained and certified to support others.
Libraries for Health: Innovative programs like "Libraries for Health" have placed peer specialists in non-traditional settings like rural public libraries. In towns where the library is the only community hub with reliable air conditioning and internet, these peers become the frontline of the mental health system.
Limitations: While peers provide vital emotional support and navigation, they cannot diagnose, prescribe, or treat severe pathology. They are a supplement to, not a substitute for, clinical care. However, in many Texas counties, they are the only resource available.
Geographic Disparities – The Rural-Urban Divide
Texas is often described as two states: the booming, connected urban archipelago and the vast, isolated rural sea. The experience of accessing therapy differs radically depending on which Texas one inhabits.
The Rural Crisis: Isolation and the Digital Divide
Rural Texas is facing a demographic and healthcare crisis. The population is aging, hospitals are closing, and connectivity is unreliable.
Maternity and Mental Health Deserts: More than 90 rural hospitals have stopped delivering babies, creating "maternity deserts." This has a direct impact on maternal mental health, as postpartum depression screenings often occur at obstetric follow-ups. If a mother has to drive 70 miles for a checkup, she is less likely to go, and her mental health needs are missed.
The Broadband Barrier: Telehealth is often touted as the panacea for rural shortages. However, its efficacy relies on high-speed internet. In 2026, the "digital divide" remains a significant determinant of health. The "Rural Health Transformation Program," funded by the "One Big Beautiful Bill Act" (OBBBA) passed in July 2025, has earmarked nearly $1 billion for Texas rural health systems, including broadband infrastructure. Yet, infrastructure projects take time. For a rancher in West Texas with satellite internet that cuts out during storms, a video therapy session is often technically unfeasible.
Audio-Only Necessity: Recognizing this reality, Texas policy has had to adapt. The state has extended waivers that allow reimbursement for audio-only (telephone) telehealth services. This is a lifeline for rural seniors who may not have smartphones or broadband but do have landlines. It ensures that lack of video capability does not equal lack of care.
The Border Region: A Distinct Ecosystem
The Texas-Mexico border region represents a unique intersection of challenges.
Trauma and Stress: The region is a focal point for immigration debates and enforcement. Residents live in a highly militarized environment, which can act as a chronic stressor. Furthermore, many families have mixed immigration status, leading to constant anxiety about deportation and family separation.
Colonias: Thousands of Texans live in "colonias"—unincorporated settlements along the border that often lack basic infrastructure like potable water, paved roads, and electricity. In these communities, the hierarchy of needs pushes mental health to the bottom. However, research conducted in 2024-2025 in South Texas colonias reveals a high prevalence of despair, anxiety, and heat-related stress.
Bi-National Care: Historically, many border residents crossed into Mexico for affordable medical and psychiatric care. However, border security fluctuations and violence in Mexican border cities can disrupt this informal safety valve, forcing residents back into the under-resourced Texas system.
The Urban Paradox
In the major metros—Houston, DFW, Austin—the problem is not the absence of providers, but the congestion of the system.
Saturation and Cost: While providers exist, the cost of living in these cities drives up practice overhead. Consequently, urban therapists are the most likely to opt out of insurance networks. An Austin resident may have 500 therapists in their zip code, but if they rely on insurance, they may still face a 3-month waitlist for an in-network provider.
Traffic as a Barrier: In sprawling metros like Houston, the physical time required to attend therapy is a barrier. A 50-minute session might require 2 hours of commute time. This makes telehealth preferred, but also highlights the importance of neighborhood-based community clinics, which are often lacking in rapidly gentrifying areas.
Specific Vulnerable Populations
The aggregate data masks the deep disparities affecting specific groups. In 2026, the system fails different populations in different ways.
The Hispanic Mental Health Gap
Hispanics are now the plurality of the Texas population, yet the mental health system remains culturally mismatched.
Representation Gap: While Hispanics make up over 40% of the population, they constitute only ~8% of the psychology workforce. This "concordance gap" is critical. Therapy is a linguistic and cultural process. A patient struggling to articulate emotional nuance in their second language to a therapist who does not understand the cultural concept of familismo is at a profound disadvantage.
Stigma: Cultural stigma remains a potent barrier. Mental illness is often viewed through a lens of privacy or spiritual failure rather than medical necessity. The concept of aguantar (endurance/resilience) can lead to the suppression of symptoms until they become unmanageable.
Uninsured Rates: Hispanic Texans have the highest uninsured rates of any major demographic group, compounding the cultural barriers with financial ones.
Youth: A Crisis in the Classroom
Texas youth are facing rising rates of anxiety, depression, and suicidality.
School-Based Limitations: With one of the highest student-to-counselor ratios in the country, Texas schools are ill-equipped to handle complex pathology. Counselors are often overburdened with academic testing and scheduling duties.
The TCMHCC Success: A bright spot in 2026 is the Texas Child Mental Health Care Consortium (TCMHCC). This state-funded initiative connects universities (like UT Southwestern and Baylor College of Medicine) with local school districts via telehealth. Programs like TCHATT (Texas Child Health Access Through Telemedicine) allow a student in crisis to be assessed by a psychiatrist via iPad in the school nurse's office, bypassing the months-long wait for community care. This program has become a national model for leveraging academic resources to serve the public.
Maternal Mental Health
Untreated maternal mental health conditions (MMHCs) are a silent epidemic.
Prevalence: In 2025, nearly 13% of Texas women reported postpartum depressive symptoms.
Medicaid Extension: Texas recently extended Medicaid coverage for pregnant women to 12 months postpartum. This is a critical policy win, allowing mothers to access therapy for a full year after birth. However, the shortage of providers who accept Medicaid means that having the card does not guarantee getting the care.
Emerging Determinants – Climate and Chemistry
In 2026, the determinants of mental health have expanded beyond the social and economic to the environmental and chemical.
The Heat-Health Nexus
Texas is on the front lines of climate change, with summers now consistently featuring "heat domes" that trap high pressure and extreme temperatures for weeks.
Physiological Impact: Research published in 2024 and 2025 has established a direct clinical link between extreme heat and mental health. Heat stress disrupts sleep architecture, increases cortisol levels, and impairs cognitive function.
Clinical Outcomes: Studies show that during heat waves, emergency room visits for mental health crises, including suicide attempts and manic episodes, spike significantly. Patients taking psychotropic medications like lithium or antipsychotics are at higher risk because these drugs can interfere with the body's thermoregulation, increasing the risk of heat stroke.
Psychological Toll: Beyond physiology, the heat creates a sense of entrapment. For low-income Texans without reliable air conditioning, the summer becomes a period of chronic, low-grade trauma and isolation, referred to in focus groups as a cycle of "physical stress followed by despair".
The Evolving Substance Use Crisis
The opioid crisis in Texas has mutated.
Fentanyl and Tucker's Law: Following the passage of Tucker's Law (HB 3908), Texas schools now mandate fentanyl education. Awareness has increased, but the supply chain has evolved.
The Rise of Xylazine: In 2026, the drug supply in cities like El Paso and Houston increasingly contains xylazine ("tranq"), a veterinary sedative mixed with fentanyl. Xylazine causes severe skin ulcerations and renders Naloxone (Narcan) less effective because it is not an opioid. This complicates overdose response and requires a new tier of medical and wound-care integration into substance use treatment—resources that are scarce in the state's underfunded addiction treatment centers.
The Policy and Regulatory Environment (2025-2026)
The 89th Texas Legislative Session and recent federal actions have reshaped the regulatory landscape.
Telehealth and Payment Parity
Texas has moved to solidify the gains made during the pandemic. HB 1052 mandated that state-regulated health plans cover telehealth services, and critical payment parity laws have been enacted to ensure providers are reimbursed at the same rate for video visits as in-person visits. This economic stability is crucial for encouraging providers to invest in telehealth infrastructure. However, the expiration of federal Medicare flexibilities in late 2025 regarding the "in-person requirement" for prescribing controlled substances remains a friction point, complicating care for patients needing stimulants for ADHD or benzodiazepines for anxiety.
The IMD Exclusion Battle
Texas hospitals continue to fight the federal Institutions for Mental Diseases (IMD) exclusion, which prohibits Medicaid from paying for care in psychiatric facilities with more than 16 beds for adults aged 21-64. This antiquated rule severely limits the state's capacity to treat indigent adults in crisis. Texas has sought waivers to bypass this, arguing that allowing Medicaid funds to follow the patient would incentivize the building of new psychiatric beds, alleviating the backlog in county jails where many mentally ill Texans currently reside.
Conclusion and Strategic Outlook
As Texas navigates 2026, the state of mental health access is a testament to the friction between immense potential and entrenched structural inertia. The state possesses the medical expertise, the academic institutions, and the economic resources to build a world-class behavioral health system. Initiatives like the Texas Child Mental Health Care Consortium and the push for collaborative care demonstrate that innovation is possible.
However, these points of light are currently insufficient to illuminate the vast shadow cast by the uninsured rate and the workforce shortage. The fundamental mathematics of the system—too few providers, too many uninsured, and too many barriers to entry—remain unsolved.
For the commercial psychotherapy practice, this landscape presents both a challenge and a moral imperative. The market is characterized by high demand and high acuity. Patients entering therapy in 2026 are likely to carry a heavier burden of complexity—compounded by economic stress, climate anxiety, and delayed care—than in previous decades. Navigating this environment requires not just clinical excellence, but a deep understanding of the systemic forces shaping the patient's journey before they ever walk through the door.
Strategic Recommendations for Stakeholders
For Policymakers: Prioritize closing the coverage gap. Whether through a conservative "Texas Way" waiver or traditional expansion, the sheer volume of uninsured adults is the single greatest drag on the system's efficiency and the state's economic productivity.
For Insurers: Genuine parity enforcement is non-negotiable. Network adequacy must be measured by appointment availability, not just lists of names.
For Educational Institutions: The pipeline must be widened at the residency and internship level. Funding for paid social work internships and expanded psychiatry residencies in rural hospitals is essential to redistribute the workforce.
For Providers: Embrace integrated care and telehealth. The solo practitioner model is becoming increasingly difficult to sustain for the average Texan. Models that embed therapy into primary care, schools, and community hubs represent the future of accessible delivery.
The story of Texas mental health in 2026 is unfinished. It is a narrative of a state straining against its own limitations, where the resilience of its people is tested daily by a system that has yet to catch up to their needs.
Extreme Heat and Mental Health Impact (Baylor Scott & White Health Newsroom)
First Detection of Xylazine in Texas Wastewater and Its Association with Fentanyl Use - NIH (PMC)
New Census Data: Texas Has Worst Uninsured Rate in US (Cover Texas Now)
Insurance coverage and parity for mental health and substance use disorder services (TDI)
Verify Which Health Plans Are Exempt From Prompt Pay Laws - Texas Medical Association
Mental Health Care Health Professional Shortage Areas (HPSAs) | KFF State Health Facts
Peer support could fill gaps in rural mental health coverage, but low pay challenges sustainability
Rompiendo Barreras: Dismantling Barriers to Latino Mental Health Care | UnidosUS
Texas Statewide Behavioral Health Strategic Plan: Progress Report - Fiscal Year 2025 (Texas HHS)
Explore Postpartum Depression in Texas | AHR - America’s Health Rankings
How heat affects the mind - American Psychological Association
State Telehealth Laws and Reimbursement Policies Report, Fall 2025 - CCHP